Next: Discussion and conclusions
Up: The Long-Term ST Database:
Previous: Introduction
The LTST DB contains 24-hour ambulatory records selected from Holter recordings
obtained in routine clinical practice settings in Europe and in the United
States between 1994 and 2000. Contributions were made from the BIDMC,
ICP, Brigham and Women's Hospital (Boston),
and Duke University Medical Center (Durham). The records were
collected to model real-world clinical conditions as far as possible
with or without known coronary artery disease while containing significant
number of ischemic and non-ischemic ST events. Analog records were
made using standard AECG recorders. Since AECG recorders preserves
frequency content in the signals typically up to 30 Hz, or to 45 Hz
in best cases, we digitized the records at 128 or 250 samples per second
per channel depending on the scanning system (Marquette MARS, ICR7200,
Oxford Medilog 4-24, REMCO LP 103, ZYMED) with the resolution of 12 bits.
After resampling the records to unique sampling
frequency of 250 samples per second and adjusting amplitude scale to
200 ADC units per mV, the records were preprocessed [1].
Trends of the derived
features, original ECG data and clinical informations formed the basis for
selecting the records. Each selected record contains significant
transient ST segment episodes corresponding to known ischemia (ischemic
ST episodes), significant non-ischemic heart-rate related transient
ST episodes, significant non-ischemic ST events due to axis shifts
(postural changes), or significant non-ischemic ST events due to
changes in QRS conduction. Some of the records contain arrhythmias such as
atrial and ventricular ectopy, atrial fibrillation, and/or atrio-ventricular
and intraventricular conduction defects. Other records were selected to
include examples of baseline ST displacement resulting from conditions
such as hypertension, ventricular dyskinesia, and effects on medications.
We also included a number of 24-hour records with proven acute myocardial
ischemia such as effort, resting, unstable, mixed, or Prinzmetal's angina
originally recorded at the ICP from which the 2-hour excerpts in the European
Society of Cardiology ST-T Database (ESC DB) were obtained. The LTST DB
contains sixty-five 24-hour two lead and fifteen three lead
ambulatory records with significant ST events annotated by human experts.
The records also provide individual QRS and rhythm annotations made by an
expert Holter scanning technician using a Marquette MARS system. Each record
is accompanied with detailed and compact clinical summary including: age
and sex; Holter report; report on other clinical investigations (if performed)
such as ventriculography, ECG stress test, thallium positron emission tomography,
echocardiography, stress echo, coronary angiography; relevant information
on patient conditions what includes history,
medications, history of arterial hypertension, previous myocardial infarction, left
ventricular function, cardiomyopathy, valve disease, electrolyte disturbances,
hypercapnia,
intraventricular conduction block, baseline ECG, final diagnosis; and technical
information about the record including recorder, leads, date and starting time of
recording.
During development of the LTST DB, it became obvious that non-ischemic ST events
such as sudden axis shifts, slow changes in QRS axis, QRS conduction changes and
slow drifts of ST level in general appear without regularity, and are thus forming
mixtures of non-ischemic ST events. For these reasons, the expert annotators
established improved annotation protocol. ST events were defined and annotated
independently in each channel. Initially, the protocol requires manual identification
of the isoelectric and J points simultaneously in all ECG leads throughout the records.
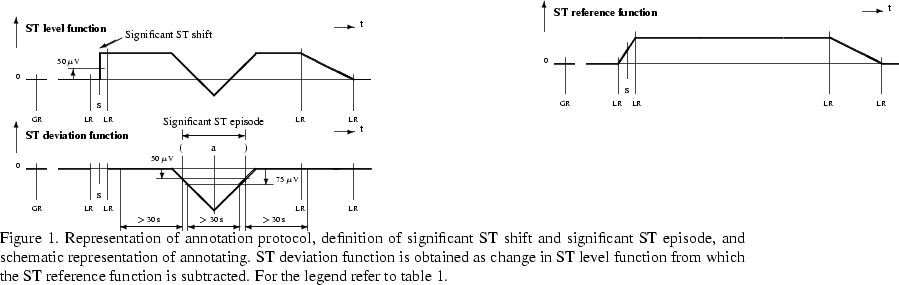
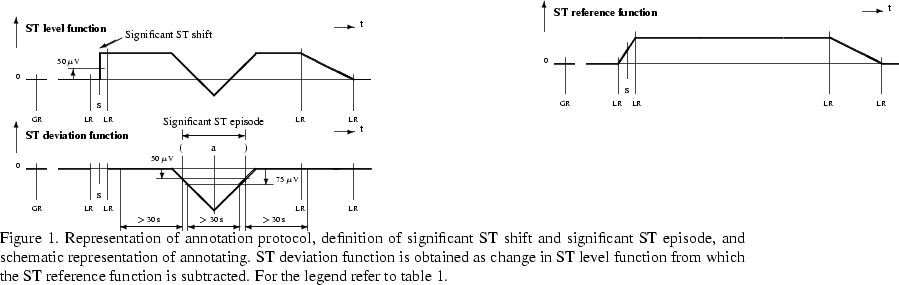
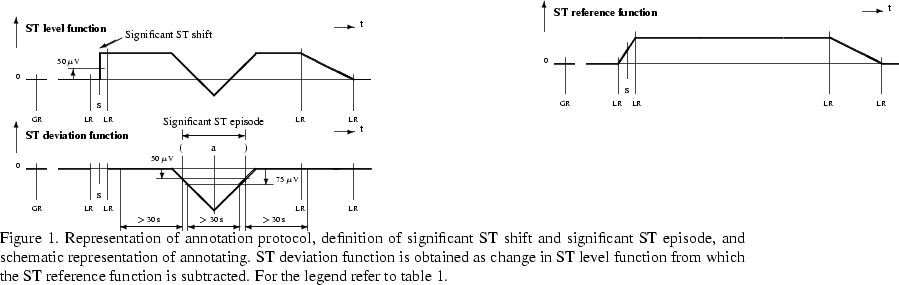
The basis for annotating ST events in each ECG lead was the ST level function
(see figure 1), which was defined as change of ST segment amplitude over time
measured 80 ms after the J point, or 60 ms after if heart rate exceeds 120 bpm.
ST segment amplitude measurements and positions of the isoelectric and J point were
obtained on time-averaged (16 seconds) heart beats derived for each ``clean'' beat
which passed the preprocessing phase. ST level function typically varies widely in
amplitude due to drifts, position changes, changes in conduction, intermittent QRS
conduction changes, heart rate changes, and ischemia. Since non-ischemic ST events
could also cause significant ( 50
50  V) shifts in ST level function, the
annotating cardiologists manually tracked the ST segment level to eliminate
these non-ischemic ST changes. The resultant ST reference function (defined
as piecewise linear function between the knot points as annotated throughout the
record by local-reference annotations in the ST level function) approximates the ST
reference level and was after that subtracted from the original ST level function
to form the ST deviation function. To successfully annotate ST events,
annotators considered ST level and ST deviation functions, original ECG signals,
time series of QRS complex and ST segment KL coefficients, and clinical information
about the patient (final diagnosis, other investigations, patient history).
Annotators also
V) shifts in ST level function, the
annotating cardiologists manually tracked the ST segment level to eliminate
these non-ischemic ST changes. The resultant ST reference function (defined
as piecewise linear function between the knot points as annotated throughout the
record by local-reference annotations in the ST level function) approximates the ST
reference level and was after that subtracted from the original ST level function
to form the ST deviation function. To successfully annotate ST events,
annotators considered ST level and ST deviation functions, original ECG signals,
time series of QRS complex and ST segment KL coefficients, and clinical information
about the patient (final diagnosis, other investigations, patient history).
Annotators also
established few characteristic categories relating to time-domain ST segment
and QRS complex morphology describing their temporal change, origin or nature:
- Change in QRS complex morphology due to slow
or sudden (postural - axis shifts) changes in the cardiac
electrical axis characterized by change in the Q, R or S wave amplitude,
or due to right or left bundle branch block, or other slow or sudden
intraventricular conduction defects characterized by bizarre and wider
QRS complex.
- Non-ischemic change in ST segment morphology due to simultaneous
slow or sudden changes in the cardiac electrical axis, due to simultaneous
slow or sudden conduction defects, or due to slow drifts. Drifts are characterized
by slow and persistent non-ischemic change in ST segment slope and shape within
longer period, and may or may not be accompanied by change in heart rate.
Category of drift includes heart-rate related diurnal changes and
effects of medication on repolarization.
- Non-ischemic heart-rate related change in ST segment morphology
characterized by change in heart rate and by non-ischemic change in ST segment
morphology within shorter period (J-point depression with positive slope,
parallel shift of ST segment compared to reference or basal ST segment).
- Ischemic change in ST segment morphology characterized by ischemic
change in ST segment morphology (flattening, down sloping, changing shape,
scooping, elevation) and may or may not be accompanied by change in heart
rate.
- Noisy ST interval characterized by consecutive ST segments which cannot
be evaluated by annotators because of noises.
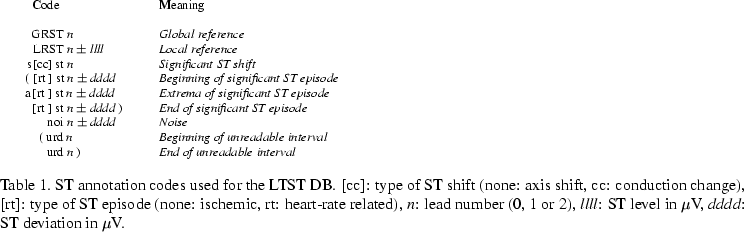
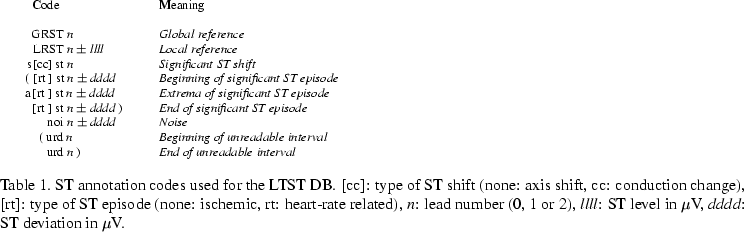
During establishing the ST reference level, the annotators first set simultaneously
for each ECG lead the global reference annotation (for the annotation codes
see table 1) representing the first stable five-minute interval after the beginning
of the record without significant variation in the ST level (basal interval).
Annotators tracked the ST segment level by a sequence of local references.
They tracked everything but ischemic and heart-rate related ST episodes, and changes
due to noises. Individual ST episodes of both types, or salvos or sequences of these
episodes, were preceded and ended by a local reference. The ST segment level was
tracked in the cases of drift, or in the cases of non-ischemic change in ST segment
morphology which had to be accompanied by simultaneous change in QRS complex
morphology and also evident in the time course of QRS complex KL coefficients.
Changes of ST level function tracked were significant ( 50
50 V) or not. Any
significant sudden-step change of ST level function which was accompanied by
simultaneous sudden-step change in QRS complex morphology was bounded by a local
reference before and after the step change and was annotated as significant
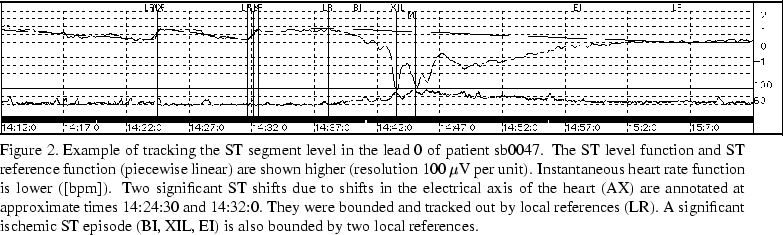
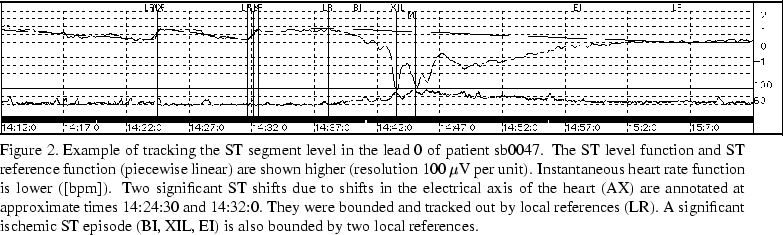
axis shift or significant conduction change according to its nature. Figure
2 shows an example of tracking the ST segment level when two significant ST shifts
and significant ST episode are present. Other ST events were annotated in the ST
deviation function. In order to be annotated, transient ST episode had to be
significant satisfying following criteria:
V) or not. Any
significant sudden-step change of ST level function which was accompanied by
simultaneous sudden-step change in QRS complex morphology was bounded by a local
reference before and after the step change and was annotated as significant
axis shift or significant conduction change according to its nature. Figure
2 shows an example of tracking the ST segment level when two significant ST shifts
and significant ST episode are present. Other ST events were annotated in the ST
deviation function. In order to be annotated, transient ST episode had to be
significant satisfying following criteria:
- An episode begins when the magnitude of the ST deviation function
first exceeds 50
 V;
V;
- The deviation must reach 75
 V or more throughout a
continuous interval of at least 30 seconds;
V or more throughout a
continuous interval of at least 30 seconds;
- The episode ends when the deviation becomes smaller than
50
 V, provided that it does not exceed 50
V, provided that it does not exceed 50 v
in the following 30 seconds;
v
in the following 30 seconds;
Significant ST episodes accompanied by non-ischemic heart-rate related change
in ST segment morphology were annotated as significant heart-rate related ST
episodes, while those accompanied by ischemic change in ST segment morphology as
significant ischemic ST episodes. Sometimes significant axis shifts or
conduction changes appeared within significant ST episodes. In these cases, they
were not tracked out, but annotated within the episodes. Sometimes significant ST
episodes appeared due to noisy ST intervals as bumps of ST deviation function.
Those shorter were annotated as noisy events at their extrema, while those
longer as unreadable intervals. Longer intervals with all heart beats rejected
during preprocessing as noisy were annotated as unreadable intervals as well.
Annotating procedure consisted from three phases. The first phase consisted from
deriving ST level functions on the basis of manually adjusted positions of
the isoelectric level and J point in time-averaged (16 seconds) heart beats
which corresponded to frequent manually set ``dummy'' annotations along the records
[1]. These positions estimated correct positions of the isoelectric
and J point for the corresponding heart beats in the centers of averaging windows.
The positions of the isoelectric level and J point for the rest of clean heart
beats were calculated by interpolating the two positions at dummy annotations
along the records. In the second phase, annotators set local references to
estimate ST reference functions and set annotations indicating significant ST
shifts. During the third phase, the ST reference functions were reviewed/corrected,
significant ST episodes were annotated automatically in the ST deviation
function, and after that manually verified/corrected. Annotators reached the
agreement on the annotations during joint meetings.
Identification and classification of transient ST episodes was accomplished
by expert cardiologists using SEMIA (semiautomatic), version 3.0 (mainly
developed by the fifth author), a special purpose graphic event-driven user
interface and signal-processing tool designed specially for this project.
It provides detailed insights into the data at multiple resolutions,
examines data at any point, presents the real ECG waveforms and trends
of ST and QRS functions, and supports manual and automatic annotation of the
records by cardiologists at different sites interacting via the Internet and
without paper tracings. New features of version 3.0, as compared to previous
version [1], are following: up to three ECG channels, user selects
``lead'', ``data'' and ``KL'' windows to form his/her own interface, dynamic
menus not permitting an annotator to go out of the required protocol and stay
consistent, several fast modes simplifying repeatable operations, memorizing
operations in the mouse buttons, and enhanced menus regarding automatic deletion
and changing attributes of annotations.
The LTST DB record files are in the WFDB format and contain detailed clinical
information for the subjects, waveform data, true QRS annotations, and ST
annotations. Each record is composed by header file
sNxxxx.hea (where N is 2 or 3 describing the number
of ECG signals and xxxx is the record number),
signal file
sNxxxx.dat,
ARISTOTLE's QRS annotation file
sNxxxx.ari,
QRS annotation atruth file
sNxxxx.atr,
ST annotation atruth file,
sNxxxx.sta, and
ST segment measurements atruth file
sNxxxx.16a.
Header files describe the format of the signal files and contain technical
information about the records, comments of expert annotators, and detailed
and compact clinical summaries for the subjects. ARISTOTLE's QRS annotation
files contain automatically derived QRS annotations and heart-beat fiducial points
which were used during preprocessing and annotating the records. QRS annotation
atruth files contain individual QRS and rhythm annotations made by expert Holter
scanning technician. ST annotation atruth files contain ST annotations (see table
1), while ST measurements atruth file contain measurements obtained
on average heart beats. These measurements were attached back to individual
heart beats in the centers of averaging windows. An annotation corresponds to
each clean beat and contains: ST amplitude measurements at the points J+80(60)ms,
J+0ms, J+20ms, J+40ms, J+60ms, J+80ms, J+100ms, and J+120ms; positions of the
isoelectric level and J point relative to the ARISTOTLE's fiducial
point; and the number of heart beats left and right to the center beat
included into the average beat.



Next: Discussion and conclusions
Up: The Long-Term ST Database:
Previous: Introduction
![]() 50
50 ![]() V) shifts in ST level function, the
annotating cardiologists manually tracked the ST segment level to eliminate
these non-ischemic ST changes. The resultant ST reference function (defined
as piecewise linear function between the knot points as annotated throughout the
record by local-reference annotations in the ST level function) approximates the ST
reference level and was after that subtracted from the original ST level function
to form the ST deviation function. To successfully annotate ST events,
annotators considered ST level and ST deviation functions, original ECG signals,
time series of QRS complex and ST segment KL coefficients, and clinical information
about the patient (final diagnosis, other investigations, patient history).
Annotators also
V) shifts in ST level function, the
annotating cardiologists manually tracked the ST segment level to eliminate
these non-ischemic ST changes. The resultant ST reference function (defined
as piecewise linear function between the knot points as annotated throughout the
record by local-reference annotations in the ST level function) approximates the ST
reference level and was after that subtracted from the original ST level function
to form the ST deviation function. To successfully annotate ST events,
annotators considered ST level and ST deviation functions, original ECG signals,
time series of QRS complex and ST segment KL coefficients, and clinical information
about the patient (final diagnosis, other investigations, patient history).
Annotators also